Supporting Patients Experiencing Poverty-Related Mental Distress
Please scroll down to view the rest of the section

Dr Uzma Haque, GP, introduces this training resource on supporting patients with poverty-related mental distress.
Explore the background to this research here:
destressproject.org.uk
Intended Learning Objectives
-
An understanding of how poverty and mental health are connected.
-
An understanding of the challenges low-income patients face and how small changes to consultation style can improve patient trust and engagement.
-
An ability to improve shared-decision making which considers a range of treatment/support options using a bio-psycho-social approach.
-
An understanding of how a team-based approach can most effectively support patients experiencing poverty-related mental distress.
Societal Distress
Dr Stephen Ward-Booth, GP and Training Programme Director of the Plymouth GP Training scheme, talks about the high levels of distress in society and the increase in the number of people presenting with mental distress in his practice.
Questions
-
What kinds of issues are people presenting with poverty-related mental distress coming to you with?
-
How are high levels of societal distress impacting on your practice as an individual and as a team?
Overprescribing
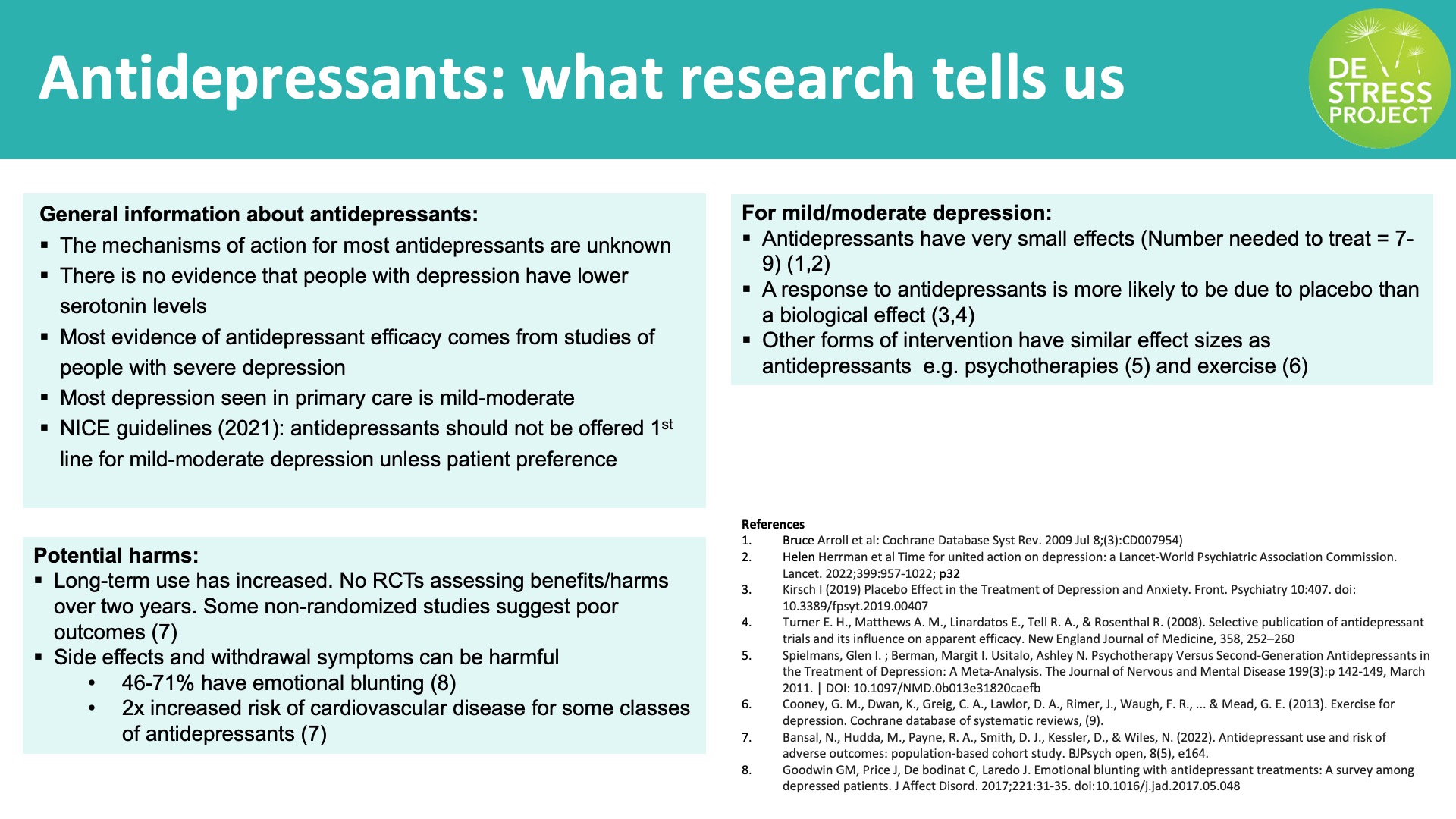
Dr Mark Horowitz gives an overview on overprescribing antidepressants. He explores the debate on how they work and the links between distress and depression including why they don’t work for some people.
Questions
-
Where do you feel your practice sits in terms of antidepressant prescribing and how has this changed in recent years?
-
How do you talk about your approach to prescribing antidepressants as a team?
-
What are your aims here as a practice?
-
-
What influences decision making on prescribing?
Question
-
How do you communicate evidence about the effectiveness of antidepressants to your patients?
Patient Experience
Dr Stephen Ward-Booth discusses some of the reasons why people find it hard to make contact with their GP.
Listen to patients discussing the challenges they faced and their experiences of consultations for mental distress.
Their stories highlight a range of approaches that made a difference to them.
Philip talks about mental health stigma and overcoming gender stereotypes to talk to his GP.
Debbie talks about the challenges she faced seeking help from her GP whilst experiencing mental distress.
Saima discusses the challenges of navigating health care when you are new to the country.
Ralph explains how helpful it has been to recognise how his mental distress relates to broader socio-economic challenges in his life.
Saiqa explains how a positive consultation means feeling valued and listened to.
Questions
-
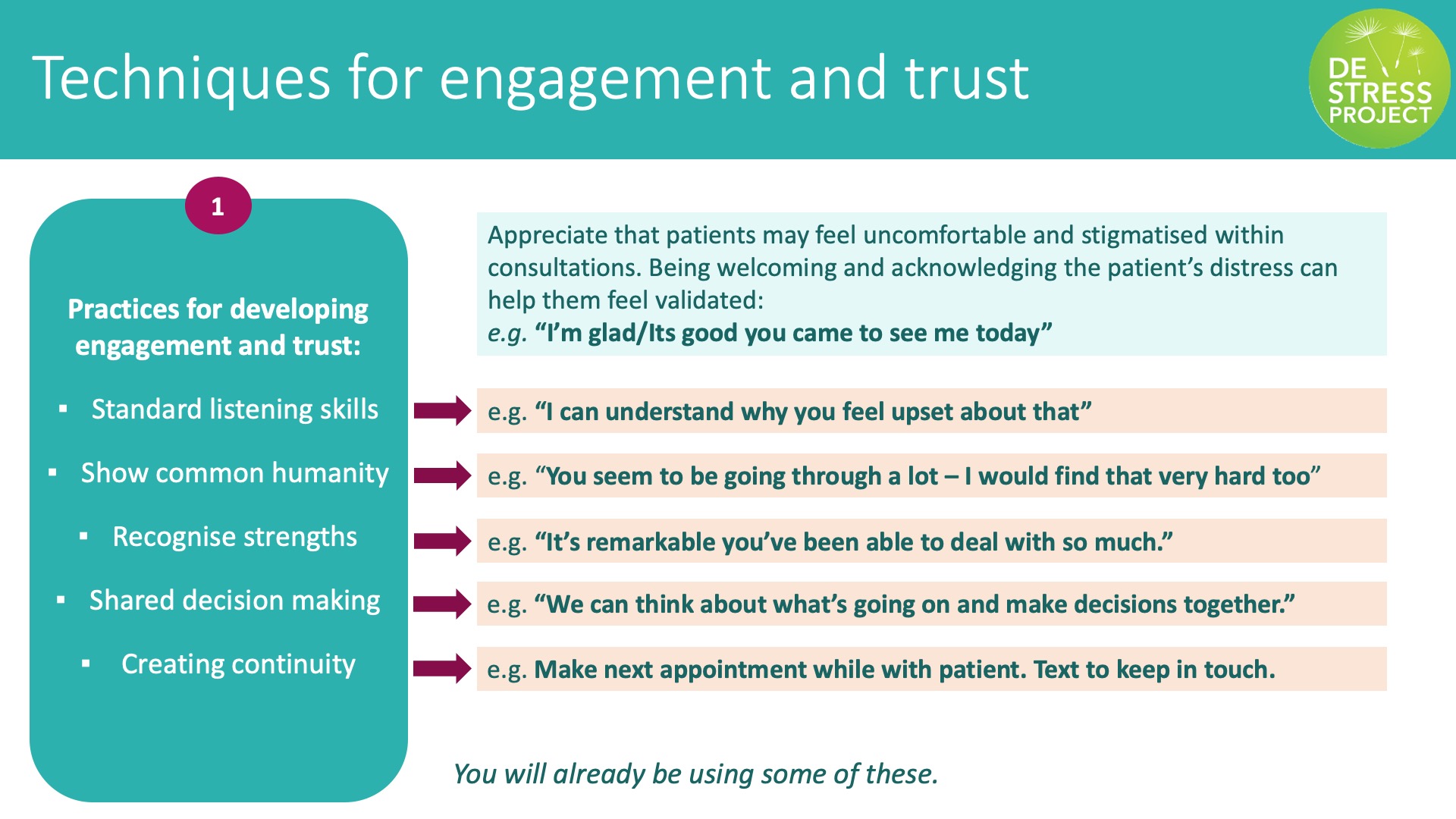
What techniques do you use that work well with people who you see presenting with poverty-related mental distress? How do you know they work?
-
Are there ways you could change your consultation approach to better support them?
From Diagnosis to Shared Understanding
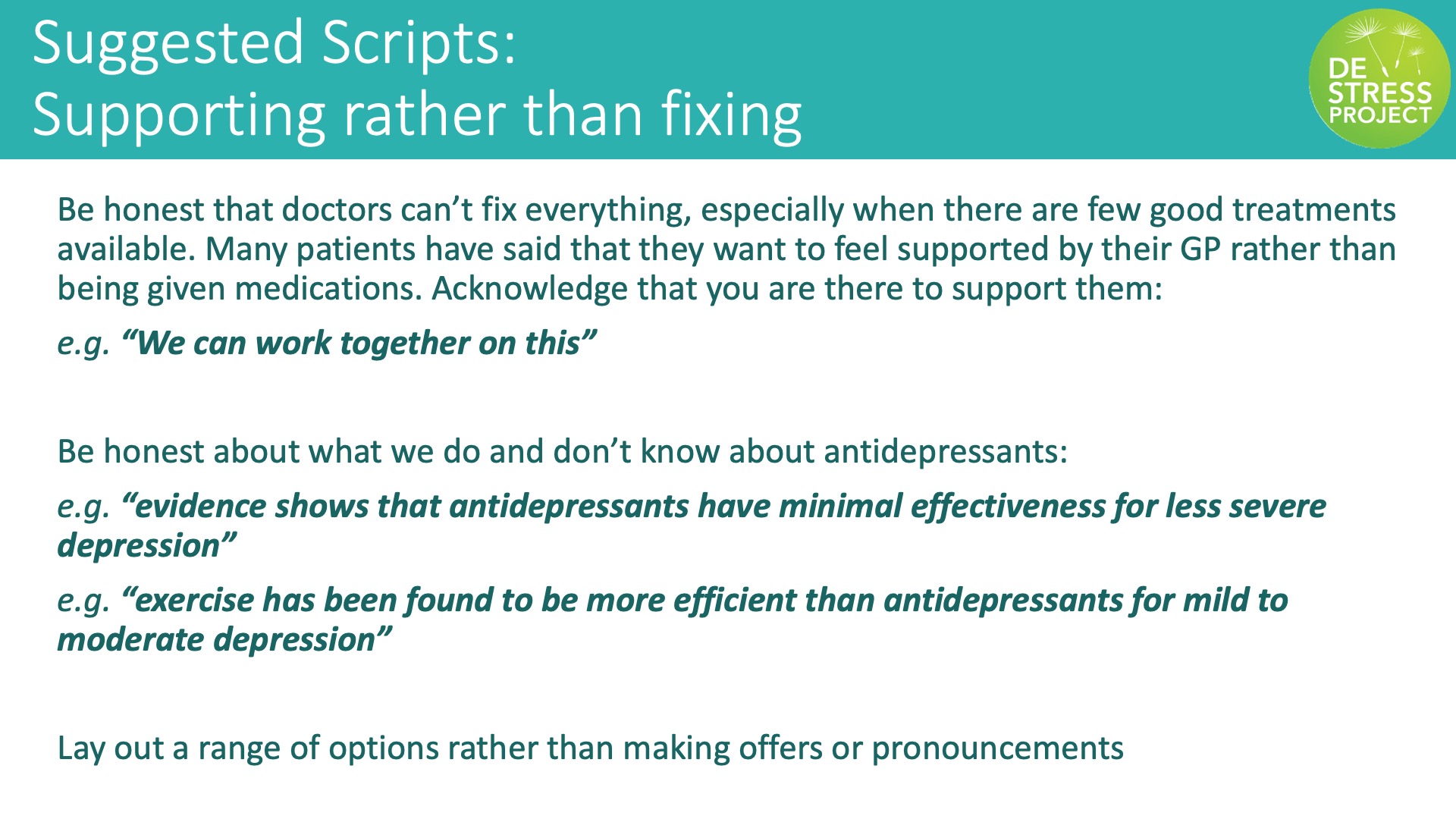
Dr Mark Horowitz outlines alternative approaches to antidepressants.
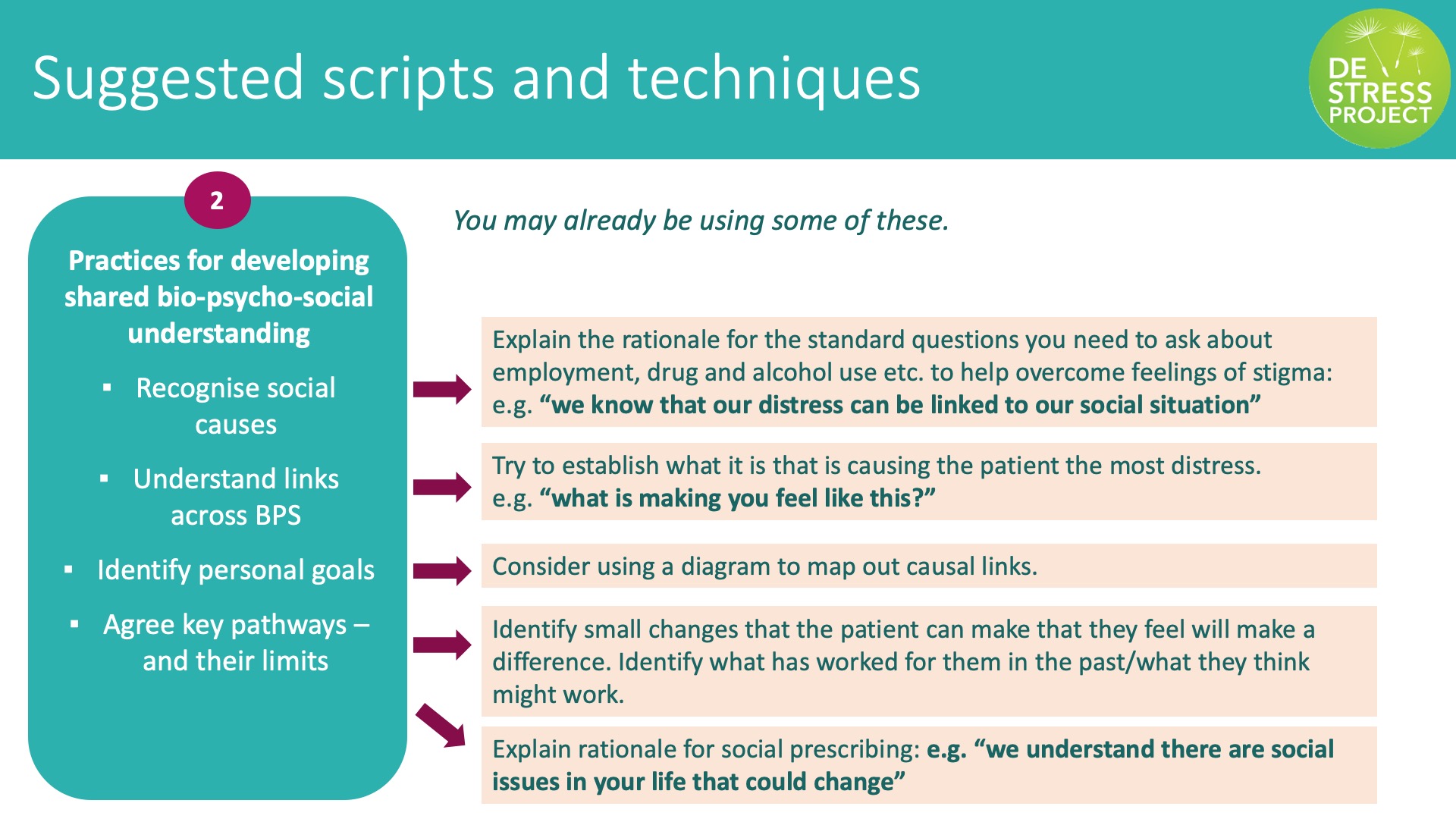
There are multiple approaches available to supporting a patient with anxiety and depression. To support them effectively it is important to consider individual circumstances and potential root causes of the distress. This section provides practical advice on how to manage consultations with patients experiencing poverty related mental distress and explore different support options.
Recommendations
When exploring management options:
-
Lay out a range of support options (including social prescribing) and give patients clear information about what each option involves whilst remaining mindful of resource limitations affecting low-income patients.
-
Raise patient awareness and understanding of the broader context in which antidepressants are being prescribed and the limited role of drugs.
Here are some things to consider in conversations with people who are experiencing mental distress due to economic disadvantage:
-
Acknowledge and validate people’s suffering through empathic listening on the whole situation. This may be what the patient wants more than the diagnosis.
-
Use a bio-psycho-social model that recognises the interconnections between physical, mental and social issues.
-
Be aware of the broader (health, social, economic) implications of a diagnosis for the patient.
-
If the patient needs a diagnosis to gain statutory support, consider demonstrating need through detailing the key symptoms.
Supporting the Patient
Dr Stephen Ward-Booth shares the approach he uses to support people presenting with poverty-related mental distress and the evidence for antidepressants.
Some patients who are experiencing mental distress might have an expectation that anti-depressants are the only and best option for them. This section explores how to address this expectation empathetically and empower your patient to address the underlying issues that are causing their distress.
Dr Mark Gabbay, Professor of General Practice, Department of Primary Care and Mental Health, University of Liverpool describes his consultation approach using empathy to empower people.
Questions
-
How would you elicit what is important to a patient when you speak to them about mental distress? E.g. cultural background; socio-economic circumstance
-
What do you find helpful in supporting a person who finds it difficult to open up in a consultation?
GP Consultation
These clips show a positive GP consultation experience. Ralph tells us what it feels like to arrive at a GP consultation and GP Elena Chantry uses a bio-psycho-social approach to empower and validate his experience.
Your Practice Team
Dr Stephen Ward-Booth shares the benefits of working with social prescribers
GP practices can vary in many ways – for example in terms of size, staffing, and available resources. The aim of this section if for you to focus on your practice and the team you have and explore as a team how you could improve the way you support individuals with poverty-related mental distress.
In this audio extract Gemma Kirby’s experiences as a social prescriber and collaboration within the practice are explored.
(Voiced by an actor)
Questions
-
Who is in your practice team? What are their roles, capabilities and capacities?
-
How do you as a team communicate and share the progress of individuals who are being supported for mental distress?
-
How could you improve follow-up processes in place to ensure that your patients are being supported by your practice team?
Thank you for taking the time to complete this training resource. We hope you found it helpful. Please do review your learning against the intended learning outcomes. This resource will remain available for you to use to refresh and renew training within your practice as appropriate.
This resource has been created through the collaboration of multiple individuals and organisations. We would like to thank all those involved in making it possible especially the funders and our excellent community partners.
The following section includes additional resources for you to explore and use to add further depth to your learning.
Intended Learning Objectives
-
An understanding of how poverty and mental health are connected.
-
An understanding of the challenges low-income patients face and how small changes to consultation style can improve patient trust and engagement.
-
An ability to improve shared-decision making which considers a range of treatment/support options using a bio-psycho-social approach.
-
An understanding of how a team-based approach can most effectively support patients experiencing poverty-related mental distress.

Destress resource produced by bluebridgeproject.co.uk
Copyright University of Exeter, UK
Published 2023
Extra Resources
Dr Mark Horowitz explores the debate on how antidepressants work and the link between distress and depression.
RCGP screencast link
Review on overprescribing
The Health Creation Alliance
Video on trauma informed practice in primary care and social prescribing by Wolseley Trust
Stopping antidepressants guidance from Royal College of Psychiatrists
Feedback
-
We would love to hear your feedback about this resource. Please fill out the short survey below:
Feedback on DeStress training


