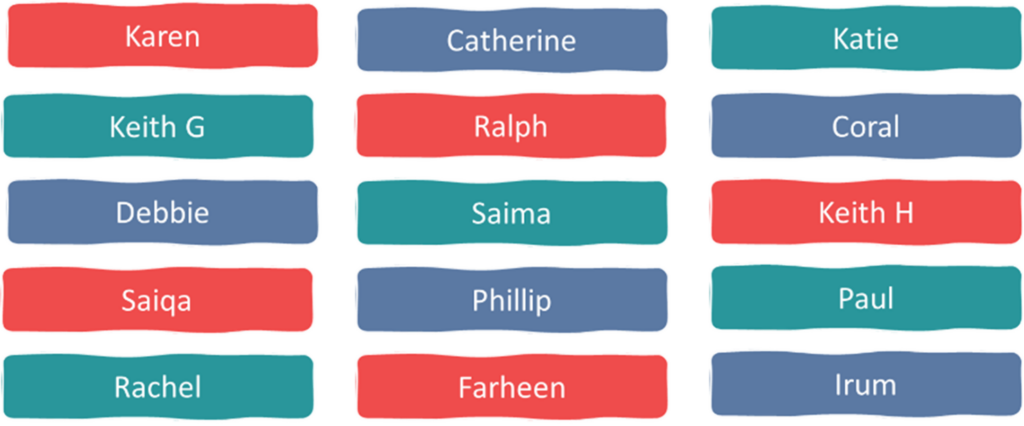
A big shout out to all the community partners above who were involved in Phase 1 of the project. We (Ralph, Debbie, Saiqa, Phillip, Saima, Keith H, Farheen and Keith G) continue to be involved both in co-creating the online training resource and disseminating the project’s key messages.
DeStress 2 - Exploring the links between poverty and mental health
Community Partners
Introducing the Destress Community Partners

Who are we and why did we get involved?
“We are a group of community partners from around the country, with lived and living experience of poor of mental health. Our experiences of medications have not always been of help to our distress and so we are highly motivated to highlight alternative and complementary options to anti-depressants, especially when the ‘blues’ or depression is caused by the long term effects of poverty and low income” Ralph
This project has offered a platform for us to share the lived experience of our journeys with mental health challenges, something many of us had not done before. Sharing our experiences of the limitations of antidepressants, the importance of a supportive GP and to promote the alternatives that have been so effective for us, has opened up the opportunity for different conversations within the GP practices.
What was the Destress experience like?
“As community partners we feel we have played a crucial role, both working with the research team to develop the training materials as well as co-delivering training to GPs and other health professionals to better identify and understand mental distress in their patients.” Farheen
“In my 31 years of being involved in patient and public engagement, I have not been involved in a project like this where we have been spread across the country and yet we have all gelled together so well. Long may it continue”. Keith H
Our online peer support ‘Drop In’ sessions
This was how we connected with each other, both community partners and the research team – and it became the space where relationships flourished and co-learning took place. We ran these sessions twice a week during the busy phase 1 training delivery stage, both daytime and evening to work around peoples’ lives. Being a ‘drop in’ allows informality, flexibility and no agenda so people could use the space and the support in whatever way worked for them at that time.
“This was an amazing resource for us, we supported each other as well as sharing and learning together, so we grew in confidence in sharing our personal stories and the training delivery. I have to also mention that we had a lot of fun too” Phillip
“The drop ins were a great help in giving us the confidence and the courage to co deliver the training and to share our personal stories. It helped us feel valued and involved.” Saiqa
“As a newcomer to the country, with a language barrier and having to learn a whole new healthcare system, I really valued the drop -in sessions where I learnt how to talk from the heart, and to share with GPs who support others like me.” Saima
What next for us?
We have collectively built confidence to use our voices and have since been involved in other research projects and proposals around deprescribing and some of us work closely with other mental health organisations. Now we are thinking beyond the project to become a group in our own right, tying together different people and different communities as partners with lived experience, and possibly approaching institutions to work together to identify where research gaps lie.
Together we have been a unifying force, and we are really proud of what we have all achieved by working together.
